WHO Media Centre
Infant and young child feeding
Fact sheet N°342
Updated January 2016
Key facts
- Every infant and child has the right to good nutrition according to the Convention on the Rights of the Child.
- Undernutrition is associated with 45% of child deaths.
- Globally in 2013, 161.5 million children under 5 were estimated to be stunted, 50.8 million were estimated to have low weight-for-height, and 41.7 million were overweight or obese.
- About 36% of infants 0 to 6 months old are exclusively breastfed.
- Few children receive nutritionally adequate and safe complementary foods; in many countries less than a fourth of infants 6–23 months of age meet the criteria of dietary diversity and feeding frequency that are appropriate for their age.
- Over 800 000 children’s lives could be saved every year among children under 5, if all children 0–23 months were optimally breastfed . Breastfeeding improves IQ, school attendance, and is associated with higher income in adult life.1
- Improving child development and reducing health costs through breastfeeding results in economic gains for individual families as well as at the national level.
Overview
Undernutrition is estimated to cause 3.1 million child deaths annually or 45% of all child deaths. Infant and young child feeding is a key area to improve child survival and promote healthy growth and development. The first 2 years of a child’s life are particularly important, as optimal nutrition during this period lowers morbidity and mortality, reduces the risk of chronic disease, and fosters better development overall.
Optimal breastfeeding is so critical that it could save over 800 000 under 5 child lives every year.
WHO and UNICEF recommend:
- early initiation of breastfeeding within 1 hour of birth;
- exclusive breastfeeding for the first 6 months of life; and
- introduction of nutritionally-adequate and safe complementary (solid) foods at 6 months together with continued breastfeeding up to 2 years of age or beyond.
However, many infants and children do not receive optimal feeding. For example, only about 36% of infants aged 0 to 6 months worldwide are exclusively breastfed over the period of 2007-2014.
Recommendations have been refined to also address the needs for infants born to HIV-infected mothers. Antiretroviral drugs now allow these children to exclusively breastfeed until they are 6 months old and continue breastfeeding until at least 12 months of age with a significantly reduced risk of HIV transmission.
Breastfeeding
Exclusive breastfeeding for 6 months has many benefits for the infant and mother. Chief among these is protection against gastrointestinal infections which is observed not only in developing but also industrialized countries. Early initiation of breastfeeding, within one hour of birth, protects the newborn from acquiring infections and reduces newborn mortality. The risk of mortality due to diarrhoea and other infections can increase in infants who are either partially breastfed or not breastfed at all.
Breast milk is also an important source of energy and nutrients in children aged 6 to 23 months. It can provide half or more of a child’s energy needs between the ages of 6 and 12 months, and one third of energy needs between 12 and 24 months. Breast milk is also a critical source of energy and nutrients during illness, and reduces mortality among children who are malnourished.
Children and adolescents who were breastfed as babies are less likely to be overweight/obese. Additionally, they perform better on intelligence tests and have higher school attendance. Breastfeeding is associated with higher income in adult life. Improving child development and reducing health costs result in economic gains for individual families as well as at the national level.1
Longer durations of breastfeeding also contribute to the health and well-being of mothers; it reduces the risk of ovarian and breast cancer and helps space pregnancies–exclusive breastfeeding of babies under 6 months has a hormonal effect which often induces a lack of menstruation. This is a natural (though not fail-safe) method of birth control known as the Lactation Amenorrhoea Method.
Mothers and families need to be supported for their children to be optimally breastfed. Actions that help protect, promote and support breastfeeding include:
- adoption of policies such as the International Labour Organization’s Maternity Protection Convention 183 and Recommendation No. 191, which complements Convention No. 183 by suggesting a longer duration of leave and higher benefits;
- the International Code of Marketing of Breast-milk Substitutes and subsequent relevant World Health Assembly resolutions;
- implementation of the Ten Steps to Successful Breastfeeding specified in the Baby-Friendly Hospital Initiative, including:
- skin-to-skin contact between mother and baby immediately after birth and initiation of breastfeeding within the first hour of life;
- breastfeeding on demand (that is, as often as the child wants, day and night);
- rooming-in (allowing mothers and infants to remain together 24 hours a day);
- not giving babies additional food or drink, even water, unless medically necessary;
- provision of supportive health services with infant and young child feeding counselling during all contacts with caregivers and young children, such as during antenatal and postnatal care, well-child and sick child visits, and immunization; and
- community support, including mother support groups and community-based health promotion and education activities.
Breastfeeding practices are highly responsive to supportive interventions, and the prevalence of exclusive and continued breastfeeding can be improved over the course of a few years.
Complementary feeding
Around the age of 6 months, an infant’s need for energy and nutrients starts to exceed what is provided by breast milk, and complementary foods are necessary to meet those needs. An infant of this age is also developmentally ready for other foods. If complementary foods are not introduced around the age of 6 months, or if they are given inappropriately, an infant’s growth may falter. Guiding principles for appropriate complementary feeding are:
- continue frequent, on-demand breastfeeding until 2 years of age or beyond;
- practise responsive feeding (e.g. feed infants directly and assist older children. Feed slowly and patiently, encourage them to eat but do not force them, talk to the child and maintain eye contact);
- practise good hygiene and proper food handling;
- start at 6 months with small amounts of food and increase gradually as the child gets older;
- gradually increase food consistency and variety;
- increase the number of times that the child is fed: 2-3 meals per day for infants 6-8 months of age and 3-4 meals per day for infants 9-23 months of age, with 1-2 additional snacks as required;
- use fortified complementary foods or vitamin-mineral supplements as needed; and
- during illness, increase fluid intake including more breastfeeding, and offer soft, favourite foods.
Feeding in exceptionally difficult circumstances
Families and children in difficult circumstances require special attention and practical support. Wherever possible, mothers and babies should remain together and get the support they need to exercise the most appropriate feeding option available. Breastfeeding remains the preferred mode of infant feeding in almost all difficult situations, for instance:
- low-birth-weight or premature infants;
- HIV-infected mothers;
- adolescent mothers;
- infants and young children who are malnourished; and
- families suffering the consequences of complex emergencies.
HIV and infant feeding
Breastfeeding, and especially early and exclusive breastfeeding, is one of the most significant ways to improve infant survival rates. However, HIV can pass from mother to child during pregnancy, labour or delivery, and also through breast milk. In the past, the challenge was to balance the risk of infants acquiring HIV through breastfeeding versus the higher risk of death from causes other than HIV, in particular malnutrition and serious illnesses such as diarrhoea and pneumonia, among HIV-exposed but still uninfected infants who were not breastfed.
The evidence on HIV and infant feeding shows that giving antiretroviral drugs (ARVs) to HIV-infected mothers can significantly reduce the risk of transmission through breastfeeding and also improve her health. This enables infants of HIV-infected mothers to be breastfed with a low risk of transmission (1-2%). HIV-infected mothers and their infants living in countries where diarrhoea, pneumonia and malnutrition are still common causes of infant and child deaths can therefore gain the benefits of breastfeeding with minimal risk of HIV transmission.
Since 2010, WHO has recommended that mothers who are HIV-infected take ARVs and exclusively breastfeed their babies for 6 months, then introduce appropriate complementary foods and continue breastfeeding up to the child’s first birthday. Breastfeeding should only stop once a nutritionally adequate and safe diet without breast milk can be provided.
Even when ARVs are not available, mothers should be counselled to exclusively breastfeed for 6 months and continue breastfeeding thereafter unless environmental and social circumstances are safe for, and supportive of, feeding with infant formula.
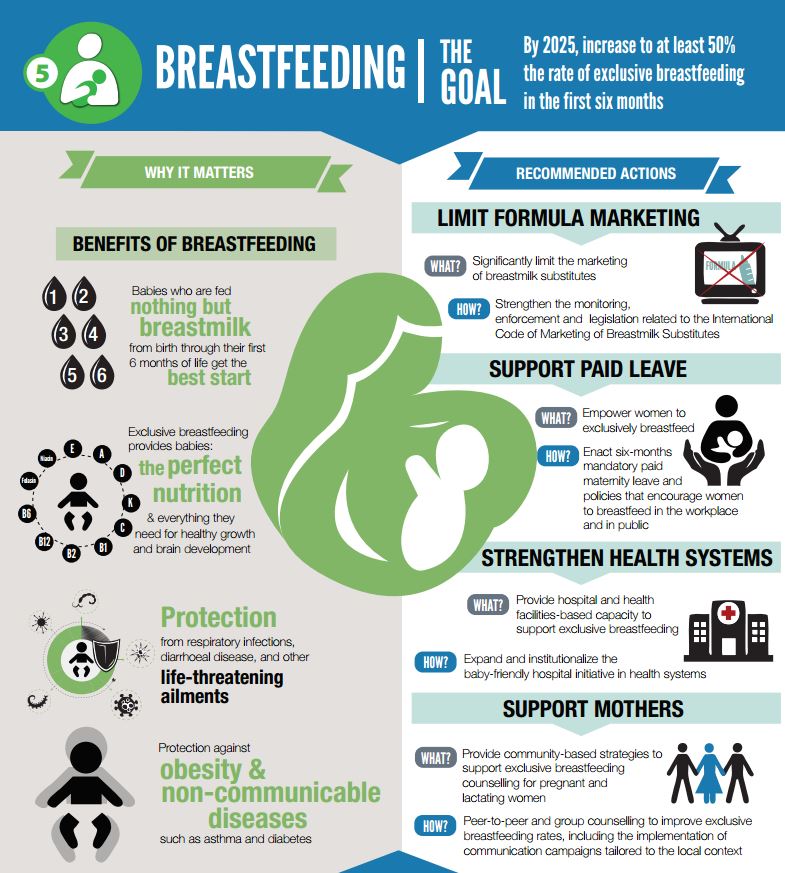
WHO’s response
WHO is committed to supporting countries with implementation and monitoring of the “Comprehensive implementation plan on maternal, infant and young child nutrition", endorsed by Member States in May 2012. The plan includes 6 targets, one of which is to increase, by 2025, the rate of exclusive breastfeeding for the first 6 months up to at least 50%. Activities that will help to achieve this include those outlined in the “Global Strategy for Infant and Young Child Feeding", which aims to protect, promote and support appropriate infant and young child feeding.
WHO has formed a Network for Global Monitoring and Support for Implementation of the International Code of Marketing of Breast-milk Substitutes and subsequent relevant WHA resolutions called NetCode. The goal of NetCode is to protect and promote breastfeeding by ensuring that breastmilk substitutes are not marketed inappropriately. Specifically, NetCode is building the capacity of Member States and civil society to strengthen national Code legislation, continuously monitor adherence to the Code, and take action to stop all violations. In addition, WHO and UNICEF have developed courses for training health workers to provide skilled support to breastfeeding mothers, help them overcome problems, and monitor the growth of children, so they can identify early the risk of undernutrition or overweight/obesity.
In addition, WHO and UNICEF have developed courses for training health workers to provide skilled support to breastfeeding mothers, help them overcome problems, and monitor the growth of children, so they can identify early the risk of undernutrition or overweight/obesity.
WHO provides simple, coherent and feasible guidance to countries for promoting and supporting improved infant feeding by HIV-infected mothers to prevent mother-to-child transmission, good nutrition of the baby, and protect the health of the mother.
1 Reference:
Series papers: Breastfeeding: The Lancet (www.thelancet.com/series/breastfeeding). Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Victora, Cesar G et al. The Lancet , Volume 387 , Issue 10017 , 475 – 490. Why invest, and what it will take to improve breastfeeding practices? Rollins, Nigel C et al. The Lancet , Volume 387 , Issue 10017 , 491 – 504
For more information contact:
WHO Media centre
Telephone: +41 22 791 2222
E-mail: mediainquiries@who.int


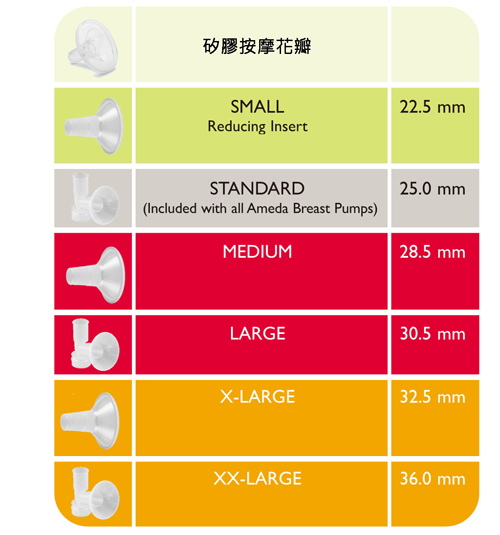
 個人化調節:
個人化調節: 獨特氣閘保護設計:
獨特氣閘保護設計: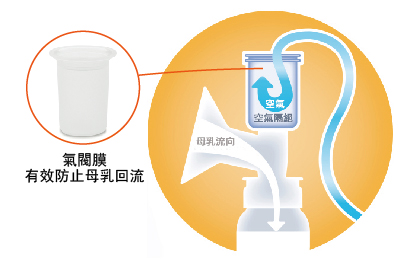
 貼服剪裁的吸罩系統:
貼服剪裁的吸罩系統: