WHO Media Centre
Infant and young child feeding
Fact sheet N°342
Updated January 2016
Key facts
- Every infant and child has the right to good nutrition according to the Convention on the Rights of the Child.
- Undernutrition is associated with 45% of child deaths.
- Globally in 2013, 161.5 million children under 5 were estimated to be stunted, 50.8 million were estimated to have low weight-for-height, and 41.7 million were overweight or obese.
- About 36% of infants 0 to 6 months old are exclusively breastfed.
- Few children receive nutritionally adequate and safe complementary foods; in many countries less than a fourth of infants 6–23 months of age meet the criteria of dietary diversity and feeding frequency that are appropriate for their age.
- Over 800 000 children’s lives could be saved every year among children under 5, if all children 0–23 months were optimally breastfed . Breastfeeding improves IQ, school attendance, and is associated with higher income in adult life.1
- Improving child development and reducing health costs through breastfeeding results in economic gains for individual families as well as at the national level.
Overview
Undernutrition is estimated to cause 3.1 million child deaths annually or 45% of all child deaths. Infant and young child feeding is a key area to improve child survival and promote healthy growth and development. The first 2 years of a child’s life are particularly important, as optimal nutrition during this period lowers morbidity and mortality, reduces the risk of chronic disease, and fosters better development overall.
Optimal breastfeeding is so critical that it could save over 800 000 under 5 child lives every year.
WHO and UNICEF recommend:
- early initiation of breastfeeding within 1 hour of birth;
- exclusive breastfeeding for the first 6 months of life; and
- introduction of nutritionally-adequate and safe complementary (solid) foods at 6 months together with continued breastfeeding up to 2 years of age or beyond.
However, many infants and children do not receive optimal feeding. For example, only about 36% of infants aged 0 to 6 months worldwide are exclusively breastfed over the period of 2007-2014.
Recommendations have been refined to also address the needs for infants born to HIV-infected mothers. Antiretroviral drugs now allow these children to exclusively breastfeed until they are 6 months old and continue breastfeeding until at least 12 months of age with a significantly reduced risk of HIV transmission.
Breastfeeding
Exclusive breastfeeding for 6 months has many benefits for the infant and mother. Chief among these is protection against gastrointestinal infections which is observed not only in developing but also industrialized countries. Early initiation of breastfeeding, within one hour of birth, protects the newborn from acquiring infections and reduces newborn mortality. The risk of mortality due to diarrhoea and other infections can increase in infants who are either partially breastfed or not breastfed at all.
Breast milk is also an important source of energy and nutrients in children aged 6 to 23 months. It can provide half or more of a child’s energy needs between the ages of 6 and 12 months, and one third of energy needs between 12 and 24 months. Breast milk is also a critical source of energy and nutrients during illness, and reduces mortality among children who are malnourished.
Children and adolescents who were breastfed as babies are less likely to be overweight/obese. Additionally, they perform better on intelligence tests and have higher school attendance. Breastfeeding is associated with higher income in adult life. Improving child development and reducing health costs result in economic gains for individual families as well as at the national level.1
Longer durations of breastfeeding also contribute to the health and well-being of mothers; it reduces the risk of ovarian and breast cancer and helps space pregnancies–exclusive breastfeeding of babies under 6 months has a hormonal effect which often induces a lack of menstruation. This is a natural (though not fail-safe) method of birth control known as the Lactation Amenorrhoea Method.
Mothers and families need to be supported for their children to be optimally breastfed. Actions that help protect, promote and support breastfeeding include:
- adoption of policies such as the International Labour Organization’s Maternity Protection Convention 183 and Recommendation No. 191, which complements Convention No. 183 by suggesting a longer duration of leave and higher benefits;
- the International Code of Marketing of Breast-milk Substitutes and subsequent relevant World Health Assembly resolutions;
- implementation of the Ten Steps to Successful Breastfeeding specified in the Baby-Friendly Hospital Initiative, including:
- skin-to-skin contact between mother and baby immediately after birth and initiation of breastfeeding within the first hour of life;
- breastfeeding on demand (that is, as often as the child wants, day and night);
- rooming-in (allowing mothers and infants to remain together 24 hours a day);
- not giving babies additional food or drink, even water, unless medically necessary;
- provision of supportive health services with infant and young child feeding counselling during all contacts with caregivers and young children, such as during antenatal and postnatal care, well-child and sick child visits, and immunization; and
- community support, including mother support groups and community-based health promotion and education activities.
Breastfeeding practices are highly responsive to supportive interventions, and the prevalence of exclusive and continued breastfeeding can be improved over the course of a few years.
Complementary feeding
Around the age of 6 months, an infant’s need for energy and nutrients starts to exceed what is provided by breast milk, and complementary foods are necessary to meet those needs. An infant of this age is also developmentally ready for other foods. If complementary foods are not introduced around the age of 6 months, or if they are given inappropriately, an infant’s growth may falter. Guiding principles for appropriate complementary feeding are:
- continue frequent, on-demand breastfeeding until 2 years of age or beyond;
- practise responsive feeding (e.g. feed infants directly and assist older children. Feed slowly and patiently, encourage them to eat but do not force them, talk to the child and maintain eye contact);
- practise good hygiene and proper food handling;
- start at 6 months with small amounts of food and increase gradually as the child gets older;
- gradually increase food consistency and variety;
- increase the number of times that the child is fed: 2-3 meals per day for infants 6-8 months of age and 3-4 meals per day for infants 9-23 months of age, with 1-2 additional snacks as required;
- use fortified complementary foods or vitamin-mineral supplements as needed; and
- during illness, increase fluid intake including more breastfeeding, and offer soft, favourite foods.
Feeding in exceptionally difficult circumstances
Families and children in difficult circumstances require special attention and practical support. Wherever possible, mothers and babies should remain together and get the support they need to exercise the most appropriate feeding option available. Breastfeeding remains the preferred mode of infant feeding in almost all difficult situations, for instance:
- low-birth-weight or premature infants;
- HIV-infected mothers;
- adolescent mothers;
- infants and young children who are malnourished; and
- families suffering the consequences of complex emergencies.
HIV and infant feeding
Breastfeeding, and especially early and exclusive breastfeeding, is one of the most significant ways to improve infant survival rates. However, HIV can pass from mother to child during pregnancy, labour or delivery, and also through breast milk. In the past, the challenge was to balance the risk of infants acquiring HIV through breastfeeding versus the higher risk of death from causes other than HIV, in particular malnutrition and serious illnesses such as diarrhoea and pneumonia, among HIV-exposed but still uninfected infants who were not breastfed.
The evidence on HIV and infant feeding shows that giving antiretroviral drugs (ARVs) to HIV-infected mothers can significantly reduce the risk of transmission through breastfeeding and also improve her health. This enables infants of HIV-infected mothers to be breastfed with a low risk of transmission (1-2%). HIV-infected mothers and their infants living in countries where diarrhoea, pneumonia and malnutrition are still common causes of infant and child deaths can therefore gain the benefits of breastfeeding with minimal risk of HIV transmission.
Since 2010, WHO has recommended that mothers who are HIV-infected take ARVs and exclusively breastfeed their babies for 6 months, then introduce appropriate complementary foods and continue breastfeeding up to the child’s first birthday. Breastfeeding should only stop once a nutritionally adequate and safe diet without breast milk can be provided.
Even when ARVs are not available, mothers should be counselled to exclusively breastfeed for 6 months and continue breastfeeding thereafter unless environmental and social circumstances are safe for, and supportive of, feeding with infant formula.
WHO’s response
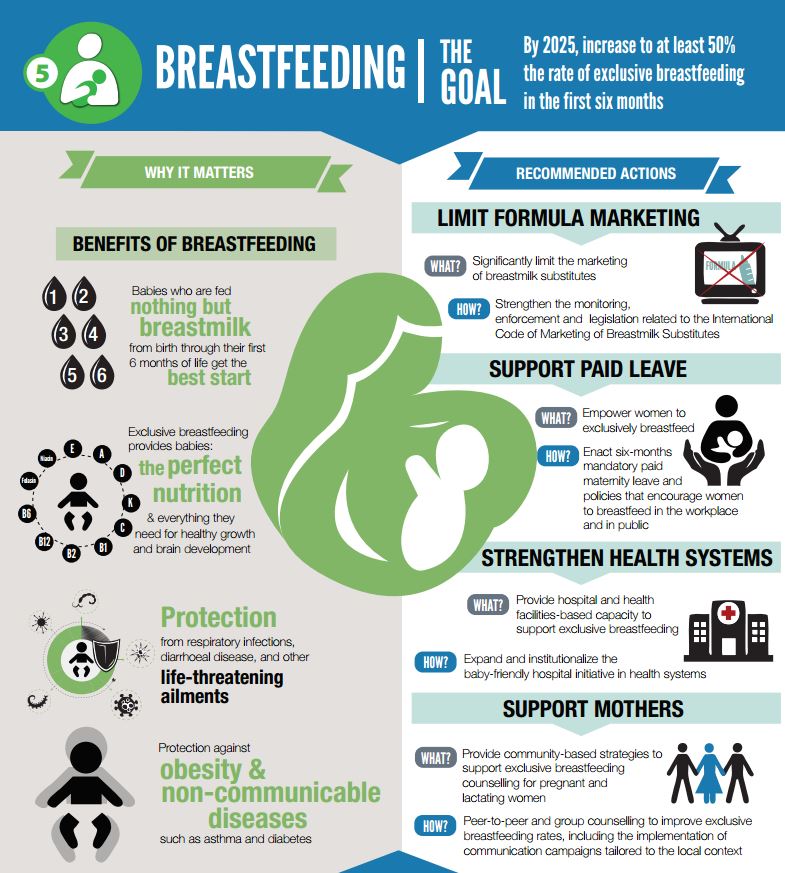
WHO is committed to supporting countries with implementation and monitoring of the “Comprehensive implementation plan on maternal, infant and young child nutrition", endorsed by Member States in May 2012. The plan includes 6 targets, one of which is to increase, by 2025, the rate of exclusive breastfeeding for the first 6 months up to at least 50%. Activities that will help to achieve this include those outlined in the “Global Strategy for Infant and Young Child Feeding", which aims to protect, promote and support appropriate infant and young child feeding.
WHO has formed a Network for Global Monitoring and Support for Implementation of the International Code of Marketing of Breast-milk Substitutes and subsequent relevant WHA resolutions called NetCode. The goal of NetCode is to protect and promote breastfeeding by ensuring that breastmilk substitutes are not marketed inappropriately. Specifically, NetCode is building the capacity of Member States and civil society to strengthen national Code legislation, continuously monitor adherence to the Code, and take action to stop all violations. In addition, WHO and UNICEF have developed courses for training health workers to provide skilled support to breastfeeding mothers, help them overcome problems, and monitor the growth of children, so they can identify early the risk of undernutrition or overweight/obesity.
In addition, WHO and UNICEF have developed courses for training health workers to provide skilled support to breastfeeding mothers, help them overcome problems, and monitor the growth of children, so they can identify early the risk of undernutrition or overweight/obesity.
WHO provides simple, coherent and feasible guidance to countries for promoting and supporting improved infant feeding by HIV-infected mothers to prevent mother-to-child transmission, good nutrition of the baby, and protect the health of the mother.
1 Reference:
Series papers: Breastfeeding: The Lancet (www.thelancet.com/series/breastfeeding). Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Victora, Cesar G et al. The Lancet , Volume 387 , Issue 10017 , 475 – 490. Why invest, and what it will take to improve breastfeeding practices? Rollins, Nigel C et al. The Lancet , Volume 387 , Issue 10017 , 491 – 504
For more information contact:
WHO Media centre
Telephone: +41 22 791 2222
E-mail: mediainquiries@who.int
- Have a written breastfeeding policy that is routinely communicated to all health care staff.
- Train all health care staff in the skills necessary to implement this policy.
- Inform all pregnant women about the benefits and management of breastfeeding.
- Help mothers initiate breastfeeding within the first hour of birth.
- Show mothers how to breastfeed and how to maintain lactation even if they are separated from their infants.
- Give newborn infants no food or drink other than breast milk, unless medically indicated.
- Practice rooming-in (allow mothers and infants to remain together) 24 h a day.
- Encourage breastfeeding on demand.
- Give no artificial nipples or pacifiers to breastfeeding infants.
- Foster the establishment of breastfeeding support groups and refer mothers to them on discharge from hospital.
Fourth edition published in 2010 by UNICEF, WHO, UNESCO, UNFPA, UNDP, UNAIDS, WFP
and the World Bank.
Facts for Life can be found at www.factsforlifeglobal.org. The website will be updated regularly and links to an interactive site for posting comments, sharing experiences and materials and discussions on relevant issues.
Translated into Chinese and modified by PB Care Company Limited on 26th Nov 2015 in Hong Kong
Breastmilk alone is the best food and drink for an infant for the first six months of life. No other food or drink, not even water, is usually needed during this period.
在孩子出生到六個月內,以純母乳餵養孩子。
人類母乳(Human Milk)是孩子們最好的食物。母乳幫助孩子生長,發育以至遠離疾病。母乳會因應各孩子各階段所需而有所變化。它會神奇地自動提供各種養份的最佳平衡給予孩子。此種只屬於個別母親與孩子之間的獨特食物。並不能由配方食物(Formula),任何奶粉(Powered Milk)或其他動物乳汁(Animal Milk)所取代。
在此生長時期的孩子,除了母乳,根本不需其他液體的補助,此也包括萬物之源 – 水份,我們稱此種餵養方式為純母乳餵養(Exclusive Breastfeeding)。值得一提,可能有母親以為天氣冷熱,空氣濕乾,是否不適宜餵哺母乳,但實際是母乳的神奇之處在因應孩子不同需要時,它就會自動變化,以應對環境變化。
如果把水份,其他液體或食物給予6個月內的孩子,即非以純母乳餵養,包括部份母乳餵養或非母乳餵養的嬰幼兒,這會非常大機會帶來以下風險:
- 不潔食物或食水,會帶來嬰幼兒腹瀉和其他感染導致死亡風險大增。
- 不進行純母乳餵養,表示孩子少膚貼膚接觸及吸吮乳房,這會減弱母嬰關係, 嬰兒減少安全感及最重要影響造乳功能。愈少貼身吸吮母親,身體便自然減少造乳,直至停止。
另外,母乳非常容易被孩子消化,反之孩子對其他動物乳汁,配方食物,奶粉都會有消化不良情況,即消化速度非常緩慢。
母乳除容易消化外,也可作為載體,把母親對疾病的免疫力及抵抗力,以抗體形式傳輸給孩子,而此種抗體,當然都是只有個別的獨特的母親才有。
母乳餵養
如果出生6個月母乳餵養嬰幼兒的發育未符理想,請注意以下事項:
- 孩子吸吮效果不好,母親可能需要幫助改善餵養技巧
- 孩子餵養次數不足,世界衛生組織 (World Health Organization) 建議必須「依需而餵」,而非「按時而餵」,相信孩子自然追求生存或生長的能力。他們有需要時自然會提出要求,而母親則按需求而滿足。不分晝夜,每24小時最少提供8次餵哺。而餵哺時間的長短也由孩子決定,相信孩子天生的能力。當他們流露出滿足的表情而甜甜入睡,自然會放開口中的乳頭,直至下一次需要而呼喚母親。
- 照顧出生時不足標準重量的孩子或早產兒,在母乳餵哺時可能需要很多暫停時間,以防止孩子嗆到。
- 孩子可能有疾病風險,需咨詢醫護人員。
- 孩子可能獲得水份或其他食物而影響母乳吸吮次數及份量。那麼母親需要純母乳餵養指引。
最後,給予零至6個月的孩子純母乳餵養還有助拉開生育間隔,這是一種自然控制生育的方法,稱為哺乳閉經避孕法。
Newborn babies should be given to the mother to hold immediately after delivery. They should have skin-to-skin contact with the mother and begin breastfeeding within one hour of birth.
產後立即開始母嬰肌膚接觸並在生命最初一小時內開始母乳餵養。
在產後立即進行膚貼膚接觸,這將有效刺激母體造乳,同時會幫助母親子宮有效收縮,減少大量出血或感染風險,並幫助排出胎盤。
初乳(Colostrum)是一種比較稠密帶黃色的乳汁,通常只會在產後數天內在母親乳房製造,初乳是新生孩子的完美食物,富含養份及充滿抗體。初乳具有孩子必須的養份及對抗感染的抗體,所以為了孩子,必須餵哺初乳。
新生兒除母乳外不需要其他食物,包括水份,如果給予水份或其他食物,這會影響母親造乳。同時孩子有腹瀉及其他感染的風險。個人化,獨特的母乳會神奇地自動根據孩子所需而自動調配養份以符合孩子在不同時間的不同需要。當然要記著「依需而餵」,而非 「按時而餵」。
如果孩子在最初餵哺期出生頭數天有吸吮問題,母親應時常把孩子放在身邊,不停幫助孩子進行,含乳頭,吸吮乳頭訓練。同時要借助泵奶器的幫助把母乳從乳房擠出。正確儲起及在孩子需要時以確保乾淨清潔的杯子餵給孩子,千萬不能用瓶子進行。母親可咨詢餵哺技巧及擠奶技巧,確保孩子能得到母乳餵哺。
對於出生時不足標準重量的孩子,如上所述其母親給予的母乳是孩子的最佳食物。 但事實這些孩子在出生首數天都可能未能可以直接從母親的乳房吸吮到母乳。 那麼擠出的母乳(Expressed Breastmilk)或捐獻母乳甚至嬰幼兒配方變成唯一食物來源。所以如何有效擠取母乳,如何儲起擠出的母乳,如何餵哺擠出的母乳,請查閱相關知識,咨詢專業人士。請注意擠出的母乳必須預熱,妥善處理及正確餵哺給孩子。最後,我們強調愛嬰醫院(baby- friendly hospital)服務,確保母親和孩子一天有24小時的全接觸,同時確保孩子獲得純母乳餵養。
Almost every mother can breastfeed successfully. Breastfeeding the baby frequently causes production of more milk. The baby should breastfeed at least eight times daily, day and night, and on demand.
差不多所有母親都可做到母乳餵哺,而更多吸吮乳房,只會引起母親製造更多母乳。強調每天需要最少8次授乳,不論白晝,黑夜及遵守 「依需而餵」而非 「按時而餵」。
母親造乳的量是根據孩子的實際需要,當孩子吸吮得多,母親同樣會製造更多母乳。差不多所有母親皆能授與足夠乳量及成功。
進行母乳餵哺,當然有如下要求的情況下:
- 母親在孩子首6個月進行純母乳餵哺
- 孩子在正確位置,正確貼上乳房,正確吸吮
- 孩子在不分晝夜的情況下得到「依需而餵」。同時母親保持授乳直至孩子滿足而離開乳房。再加上交替左右乳房授乳,即這餐由一邊授乳,下一餐由另一邊乳房交替授乳。
- 有何信號表示孩子在正確位置上授乳?
- 孩子的頭及身體成一直線
- 孩子緊貼母親身體
- 孩子的整個身體正面向著母親
- 孩子是放鬆的,開心的及正在吸吮
- 把孩子放在不正確位置會帶來什麼後果?
- 導致母親乳頭破損及一碰就疼痛
- 孩子不能獲取足夠母乳
- 孩子拒絕被餵吮
有何信號表示孩子是被正確餵食母乳?
- 你可以在孩子上唇上看到母親較多的乳暈
- 孩子的嘴部是闊大張開的
- 孩子的下唇是向外翻開的
- 孩子的下巴是貼在母親的乳房上
有何信號表示孩子吸吮良好?
- 孩子表現長及深的吸吮
- 孩子相脥鼓脹成圓形
- 當吃飽後孩子會自動放開乳房
一般而言,母親授乳時不應感到痛楚。如果有此情況,請尋求相關咨詢。請緊記生產後盡快進行授乳,一天廿四小時授乳不少於8次,授乳愈多,愈能刺激母親製造更多母乳。努力實行孩子首6個月的純母乳餵哺。相信很多母親擔憂害怕自己乳量不足或以為自己乳質不好而添加水份或其他食物與孩子,那正正是導致乳量不足的原因。因愈少吸吮,母體自然少造乳,直至停止。孩子便得不到母親給予的最貴重禮物,足以後悔一生。請尋求專業咨詢及預早作心理,生理準備實行純母乳餵哺。
Breastfeeding helps protect babies and young children against dangerous illnesses. It also creates a special bond between mother and child.
母乳餵哺能使孩子遠離很多危險疾病,同時母乳餵哺能使母親及孩子建立獨特的牽絆。
母乳是孩子一生中第一劑免疫劑,母乳能保護孩子對抗腸道,耳部及肺部感染等其他健康問題。如果在孩子出生首6個月給予純母乳餵養,這保護效果是最佳的。 現時,世上沒有其他物品可媲美母乳的功效。
進行母乳餵哺時,因親密接觸及母親對孩子的專注,可使孩子感到安全,舒適及被愛。這樣母親與孩子獨有的牽絆(Bonding)便深深植到母親及孩子的心裡。這種牽絆會影響日後母子關係及孩子自己的生長及發展。這種牽絆不可能連接父親與孩子,也不可能在其他人或物身上,所以作為父親,要認識及理解這種牽絆,同時要在身邊大力支持母親進行母乳餵哺,請尋求咨詢以了解父親及其他家人甚至親友如何支持母乳餵哺。
A woman employed away from her home can continue to breastfeed her child. She should breastfeed as often as possible when she is with the infant and express her breastmilk when they are apart so that another caregiver can feed it to the baby in a clean and safe way.
母親需要離開孩子工作時,請繼續保持母乳餵哺。
貼身母乳餵哺要堅持在母親及孩子相處時。而當母親及孩子分開時,擠奶及妥善存放母乳。請咨詢相關技巧及最佳做法,以保持優質母乳以備孩子所需。
在室溫下 (大約20-25度) 擠出的母乳可保質達8小時之久,相對其他動物乳汁及嬰幼兒配方,一般只有兩小時的保質時間,母乳又展現一個神奇的地方,但再神奇的東西如沒有乾淨合適的工具,妥善的處理方法,也有變質的可能。
After 6 months of age, when babies begin to eat foods, breastfeeding should continue for up to two years and beyond because it is an important source of nutrition, energy and protection from illness.
當孩子6個月左右,添加固體食物,繼續母乳餵哺直至兩歲甚至更久
最後當孩子6個月之後,純母乳餵哺便可功成身退,但並非全退,而是在繼續母乳餵哺同時(不論貼身授乳或擠出授乳),遂步添加流質,半流質到固體食物以滿足孩子對營養的需求。繼續授與母乳,可繼續提供能量,蛋白質,維他命A,鐵質…等等營養與孩子。相信神奇的母乳製造程序,它會根據孩子需要,自動調配成份。當然母親要提供適當原材料給與造乳工廠,否則母親孩子可能同樣面對營養不良情況。請咨詢以了解不同時期母嬰的不同需求。最後,請緊記只要有一天繼續授乳,孩子便一天繼續受母親保護,遠離疾病。
實況報導 第342號
2015年7月
重要事實
- 根據《兒童權利公約》,每個嬰幼兒都享有獲得良好營養的權利。
- 營養不良與五歲以下兒童中45%的疾病負擔相關。
- 2013年,全球範圍內,主要由於飲食不良和反復感染,估計有1.615億名五歲以下兒童發育遲緩,5080萬名兒童體重身高比例偏低,4170萬名兒童過重或肥胖。
- 約有36%的年齡不足六個月的嬰兒得到純母乳餵養。
- 獲得有足夠營養和安全的補充食品的兒童為數不多,在許多國家,6-23個月齡的母乳餵養兒童只有不到四分之一達到了與年齡適當的飲食多樣化和餵養頻率的標準。
- 如果向0–23月齡的所有兒童進行最佳母乳餵養,每年可挽救約80萬名五歲以下兒童的生命。1
概述
營養不良估計每年造成310萬名兒童死亡,占兒童死亡總數的45%。在改善兒童生存狀況,促進兒童健康成長和發育方面,嬰幼兒餵養是一個關鍵領域。兒童生命最初兩年尤為重要,在此階段如能獲得最佳營養,可降低患病率和死亡率,減少日後罹患慢性病的風險,促使身心發育更加健全。
最佳母乳餵養至關重要,每年可挽救80萬名五歲以下兒童的生命。
世衛組織和兒童基金會建議:
- 產後一小時即開始母乳餵養;
- 生命最初6個月應進行純母乳餵養;
- 在嬰兒6個月齡時增加有足夠營養和安全的補充(固體)食品,同時持續進行母乳餵養至兩歲或兩歲以上。
然而,許多嬰幼兒都得不到最佳餵養。比如,世界範圍內,2007年至2014年只有大約36%的年齡不足六個月的嬰兒得到純母乳餵養。
建議已得到修訂,以解決感染了愛滋病毒的母親所生嬰兒的需要。現在,抗逆轉錄病毒藥物讓這些嬰兒可以獲得純母乳餵養至六個月,並持續母乳餵養至少至12個月,從而使愛滋病毒傳播風險大大降低。
母乳餵養
六個月純母乳餵養對嬰兒和母親有諸多好處。主要可防止腸道感染,對發展中國家和工業化國家都是如此。儘早進行母乳餵養(產後一小時),可防止新生兒受感染並降低新生兒死亡率。對於部分母乳餵養或非母乳餵養的嬰兒,因腹瀉和其他感染導致死亡的風險可能更大。
對於6-23月齡兒童,母乳也是能量和營養素的重要來源。母乳可提供6-12月齡嬰兒所需的一半或更多的能量,12-24月齡嬰兒所需的三分之一能量。母乳還是患兒獲取能量和營養素的重要來源,並可降低營養不良兒童死亡率。
小時候得到母乳餵養的成人出現超重或肥胖的可能性較低。得到母乳餵養的兒童和青少年在智力測試方面的成績會更好。母乳餵養還有益於母親的健康和福祉。它可降低患卵巢癌和乳腺癌風險,並且有助於拉開生育間隔(對6個月以下嬰兒進行純母乳餵養可產生激素效應,通常會導致哺乳閉經期)。這是一種自然控制生育的方法,稱為哺乳閉經避孕法。
必須支持母親和家庭對嬰兒進行最佳母乳餵養。可採取有助於保護、促進和支持母乳餵養的行動,包括:
- 實行有關政策,如勞工組織《保護生育公約》(第183號)和第191號建議(該建議補充了第183號公約,其中建議延長假期和提供更高福利);
- 《國際母乳代用品銷售守則》以及世界衛生大會隨後通過的有關決議;
- 實施愛嬰醫院行動中規定的“成功母乳餵養十步驟”,包括:
- 產後立即開始母嬰肌膚接觸並在生命最初第一小時之內開始母乳餵養;
- 按需哺乳(也就是說,無論白天和夜晚,只要嬰兒需要即可哺乳);
- 母嬰同室(讓母親和嬰兒一天24小時在一起);
- 不給嬰兒喂其他食物或飲料,甚至也不喂水,除非醫療上有需要;
- 在與照料者和幼兒的接觸過程中提供嬰幼兒餵養諮詢支援性衛生服務,比如在產前和產後護理、對健康兒童和患兒的上門巡診和免疫接種期間;
- 社區支持,包括母親支持小組和社區衛生促進和教育活動。
補充餵養
6個月齡前後,母乳即滿足不了嬰兒對能量和營養素的需要,這時必須添加補充食物以滿足這些需求。嬰兒在大約6個月齡時可以開始吃其他食物。如果嬰兒6個月左右仍不添加補充食物,或者補充不當,嬰兒生長發育就會受到影響。適當補充餵養指導原則如下:
- 持續頻繁地按需哺乳直到嬰兒兩歲或兩歲以上;
- 回應式的餵食(即直接給嬰兒餵食和幫助年齡較大的兒童進食。要耐心地慢慢餵食,鼓勵兒童而不是強迫兒童進食,對孩子說話,並保持目光接觸);
- 養成良好的衛生習慣並正確處理食物;
- 嬰兒滿6個月開始添加少量食物並隨著年齡的增長逐漸增加食物的種類;
- 逐漸實現食物的合理搭配和種類多樣化;
- 增加嬰兒餵食的次數,6-8月齡嬰兒一天餵食2-3次,9-23月齡嬰兒一天餵食3-4次,根據需要可添加1-2次輔助食物;
- 根據需要使用強化補充食物或維他命礦物質補充劑;
- 對患兒增加流食的攝入,包括增加母乳餵養的次數,並給予稀軟可口的食物。
在極端困難情況下的餵養
對於處境困難的家庭和兒童應給予特別關注和實際支持。在可能的情況下,母親和嬰兒應始終在一起,並為其提供必要的支援,使之能夠採用可選擇的最適當的餵養方法。幾乎在所有困難的情況下,母乳餵養依然是首選模式,比如:
- 低出生體重或嬰兒早產;
- 感染愛滋病毒的母親;
- 未成年母親;
- 嬰幼兒營養不良;
- 家庭發生複雜的緊急情況。
愛滋病毒與嬰兒餵養
母乳餵養,特別是早期的純母乳餵養是提高嬰兒生存率最為重要的途徑之一。然而愛滋病毒可在孕期、生產時,也可通過母乳從母親傳給孩子。過去遇到的挑戰是在通過母乳餵養使嬰兒感染愛滋病毒的風險與由於愛滋病毒以外原因(尤其是發生營養不良和諸如面臨愛滋病毒暴露危險但尚未獲得感染的非母乳餵養嬰兒罹患腹瀉和肺炎等嚴重疾病)使其面臨更高的死亡風險之間進行權衡。
有關愛滋病毒和嬰兒餵養的證據表明,對感染愛滋病毒的母親使用抗逆轉錄病毒藥物,可大大降低通過母乳餵養傳播病毒的風險並會增進母親健康。這可使感染愛滋病毒的母親的嬰兒在感染風險較低(1-2%)的情況下得到母乳餵養。因此,生活在腹瀉、肺炎和營養不良仍然屬於嬰兒和兒童常見死因國家的感染愛滋病毒的母親及其嬰兒,可以在愛滋病毒感染危險極低的情況下贏得母乳餵養帶來的好處。
世衛組織自2010年以來就建議,已感染愛滋病毒的母親應服用抗逆轉錄病毒藥物並對嬰兒進行六個月純母乳餵養,隨後適當添加輔食,並用母乳持續餵養到孩子1歲。只有在能夠獲得不包括母乳在內的營養充足的安全膳食時,才停止母乳餵養。
即便沒有抗逆轉錄病毒藥物,也應當建議母親進行六個月純母乳餵養並隨後繼續用母乳餵養,除非環境和社會狀況的安全性支援度有益於用嬰兒配方粉進行餵養。
世衛組織的應對
世衛組織致力於支援各國落實並監測2012年5月由會員國批准的《孕產婦、嬰兒和幼兒營養全面實施計畫》。該計畫包括六項目標,其中一項就是到2025年將生命最初六個月的純母乳餵養率提高到至少50%。有助於實現這一目標的活動包括《嬰幼兒餵養全球戰略》所述,後者旨在促進、保護和支持適宜的嬰幼兒餵養。
世衛組織設立了全球監測和支持實施《國際母乳代用品銷售守則》以及世界衛生大會隨後有關決議的一個網路,名為“NetCode”。該網路的目標是,通過確保禁止不當銷售母乳代用品,維護和提倡母乳餵養。具體而言,該網路正在加強會員國和民間社會的能力,強化國家制定《國際母乳代用品銷售守則》實施細則的立法工作,持續監督《守則》遵循工作,並採取行動制止一切違反行為。
此外,世衛組織和兒童基金會開發了針對衛生工作者的培訓課程,為母乳餵養母親提供技能支援,並幫助他們克服困難,監測兒童生長,從而能夠早期發現營養低下或者超重/肥胖危險。
世衛組織向國家提供了簡單、一致、可行的指導,促進並支持感染了愛滋病毒的母親改善嬰兒餵養,從而預防母嬰傳播,使小兒具備良好營養,並保護母親健康。











